Abstract

Background:Clinicians are frequently faced with the choice of choosing between several different anticoagulants for a variety of indications. While there is a large body of evidence to help choose between direct oral anticoagulants (DOAC) and other agents, choosing between DOACs is a more difficult decision due to lack of head-to-head comparisons. It is likely that all DOACs are not equal in terms of safety and some may be better suited than others for individual patients based on their risk factors for different complications. Intracranial hemorrhage (ICH) is arguably the greatest safety concern with using oral anticoagulants. We hypothesized that not all DOACs are equivalent in their risk of ICH. Most prior meta-analyses have examined the risk of ICH with DOACs using only trials where non-valvular atrial fibrillation (NVAF) was the indication for anticoagulation, and a few have used trials where venous thromboembolic (VTE) disease was the indication. We are not aware of any prior meta-analyses that have combined data from trials across indications. Therefore, we aimed to evaluate the risk of intracerebral hemorrhage by performing a comprehensive traditional and network meta-analysis using data from trials across indications for anticoagulation including NVAF, VTE, and thromboprophylaxis.
Study Design: Systematic review and traditional and network meta-analyses
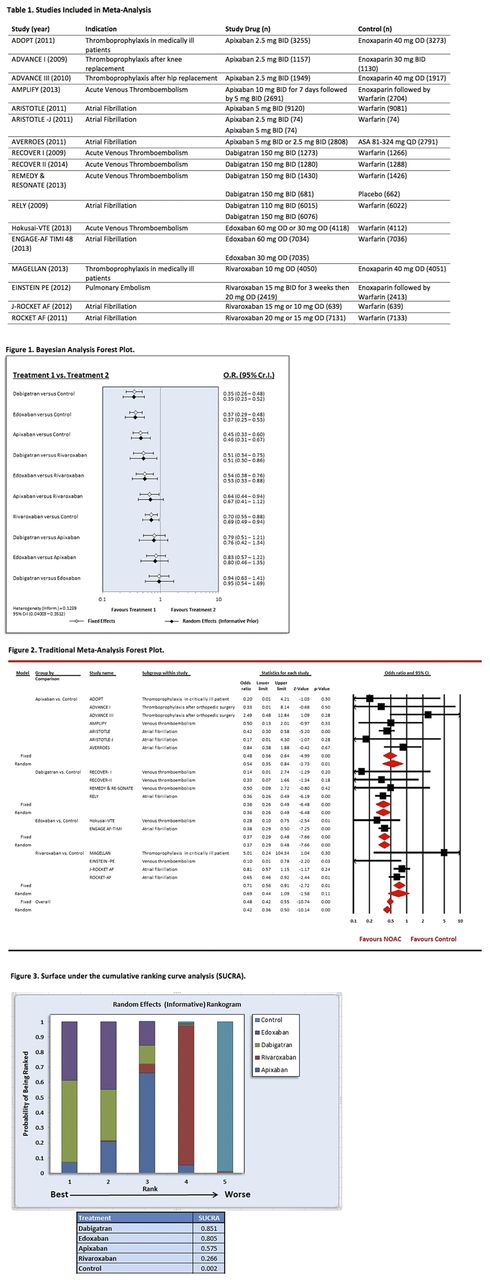
Methods: PubMed/MEDLINE, EMBASE, and the Cochrane Library were searched from inception to January 2017. Studies were eligible for inclusion if they met the following criteria: 1) phase II or III randomized controlled trial, 2) compared rivaroxaban, apixaban, edoxaban, or dabigatran to control, 3) reported intracranial hemorrhage, and 4) full-text article was available (abstracts were not included). Bayesian and conventional meta-analysis were performed to compare DOACs to control agents (warfarin, heparin, or anti-platelet agents). The primary outcome was intracranial hemorrhage. Estimates were reported as random-effects odds ratios (OR) with 95% credible intervals (Cr. I) for network analyses and OR with 95% confidence intervals (CI) for conventional analyses. DOACs were ranked based on the surface under the cumulative ranking curve analysis (SUCRA) with higher values reflecting greater safety of the drug.
Results: 17 studies (Table 1) were included in the meta-analysis (7 for apixaban, 4 for rivaroxaban, 4 for dabigatran, and 2 for edoxaban), enrolling 122,608 patients in total for safety analysis (67,875 DOAC group; 54,733 control group). Bayesian analysis showed that dabigatran and edoxaban had a reduced risk of ICH compared to rivaroxaban (OR 0.56, Cr. I 0.30-0.86 and OR 0.53, Cr. I 0.33-0.88, respectively). Bayesian analysis failed to demonstrate further significant differences between DOACs (Figure 1). Traditional meta-analysis showed that, categorically, the DOACs reduced the risk of ICH (OR 0.42, CI 0.36-0.50; p <0.01). Individually, dabigatran (OR 0.36, CI 0.26-0.49; p <0.01), edoxaban (OR 0.37, CI 0.29-0.48; p <0.01), and apixaban (OR 0.54, CI 0.35-0.84; p = 0.01) but not rivaroxaban (OR 0.69, CI 0.44-1.09; p= 0.11) had a reduced risk of ICH (Figure 2). Ranking probability ranked dabigatran as the safest drug (SUCRA 85.1%), followed by edoxaban (SUCRA 80.5%) and apixaban (SUCRA 57.5%) (Figure 3).
Conclusions: Individual DOACs carry different risk of ICH and one may consider the differences when choosing between them. Dabigatran was the safest choice among DOACs in terms of risk of ICH, and both dabigatran and edoxaban were safer than rivaroxaban. Our data reaffirm several prior meta-analyses in NVAF showing that dabigatran is safer than rivaroxaban and that DOACs categorically have a reduced risk of ICH compared to alternative anticoagulants. Our data differ in that rivaroxaban did not have a statistically significant reduction in ICH risk, likely due to the inclusion of a trial in which enoxaparin was the comparator to rivaroxaban. To our knowledge, ours is the first meta-analysis to compare the risk of ICH among DOACs using data from across indications for anticoagulation.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal